Role of coronary artery calcium score in risk prediction and therapy guidance of asymptomatic individuals
█ Review
DOI: 10.26430/CHUNGARICA.2020.50.5.324
Authors:
Judit Simon1, Lili Száraz1, Béla Merkely1, Pál Maurovich-Horvat1,2
1MTA-SE Lendület Cardiovascular Imaging Research Group, Heart and Vascular Center, Semmelweis University, Budapest
2Medical Imaging Centre, Semmelweis University, Budapest
Summary
Coronary CT angiography (CCTA) has emerged as a gatekeeper to rule out coronary artery disease (CAD), due to its high sensitivity and negative predictive value. Prior to CCTA a native calcium screening scan is acquired, which provides additional information about the coronary artery anatomy and cardiovascular risk prediction by measuring coronary artery calcification (CAC).
Based on large population-based and cohort studies, zero CAC score is linked to low probability of cardiovascular events in the future. Moreover, zero CAC score is superior in the discrimination and risk reclassification when compared with other cardiovascular risk factors. CAC score can also help to identify those who are less likely to benefit from statin pharmacotherapy.
Since CAC score has an important role in risk stratification and it is a cheap and widely accessible non-invasive imaging modality, the major guidelines have already incorporated CAC score for risk prediction and therapy guiding. However, these guidelines give slightly different recommendations. Therefore, this review aimed to introduce the CAC measurement and to summarize the prognostic role of CAC scoring in individualized risk prediction and guiding preventative therapies.
ISSUE: CARDIOLOGIA HUNGARICA | 2020 | VOLUME 50, ISSUE 5
Introduction
Coronary artery disease (CAD) is a pathological process characterized by atherosclerotic plaque accumulation in the coronary arteries, which may lead to coronary luminal narrowing and ischemia (1). CAD is the most prominent cause of morbidity and mortality in Western societies, accounting for approximately 7.4 million (13%) deaths per year (2). Since many CAD patients are asymptomatic, the first manifestation is generally myocardial infarction or sudden cardiac death (3). Therefore, there is an emerging need for improved screening tools for subclinical coronary atherosclerosis, which is a strong predictor of future adverse cardiovascular events (4–7). With the help of non-contrast enhanced low dose cardiac computed tomography (CT) scans, we can quantify the amount of coronary artery calcification (CAC). CAC scoring is a robust method to detect and quantify CAD particularly in those without any symptom (8). This review aimed to summarize the prognostic role of CAC scoring in individualized risk prediction and guiding preventative therapies.
Detection of coronary artery calcification
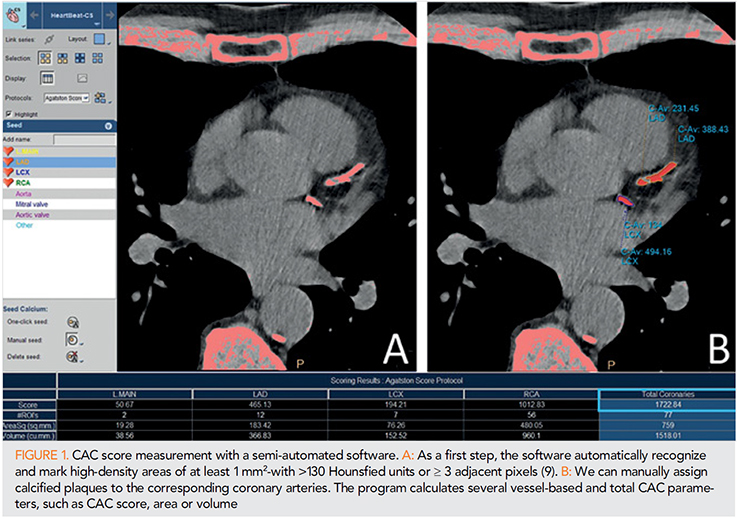
Several CAC scoring systems have been described. Among them, the Agatston score is considered as the gold standard for the quantification of CAC. Agatston score is based on the weighted density score given to the highest attenuation value (HU) multiplied by the area of the calcification speck (9). This scoring system has been adapted to the current multidetector CT, which is still the most widely used imaging modality to detect and calculate CAC score (10). Representative example of a CAC score measurement can be seen in Figure 1.
Beyond Agatston score, calcium volume score and relative calcium mass score can be used for the quantification of the extent of coronary artery calcification. Calcium volume score has proven to be the most robust and reproducible method (11). It is calculated by multiplying the number of voxels with calcification by the volume of each voxel, including all voxels with an attenuation >130 HU. However, this method is particularly sensitive to the partial volume effect. Relative calcium mass score is calculated by multiplying the mean attenuation of the calcified plaque by the plaque volume in each image, thus reducing the variation caused by the partial volume. The absolute calcium mass score uses a correction factor based on the attenuation of water (11).
Prognostic value of CAC score
Several population-based and cohort studies have investigated the prognostic value of CAC score in the prediction of CAD.
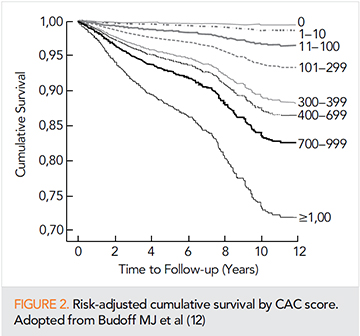
In 2007 Budoff et al. reported that based on their large cohort study of 25,253 asymptomatic individuals, CAC was an independent predictor of mortality after adjustment for age, sex, ethnic background, smoking, diabetes mellitus, positive family history for premature CAD, hypertension and hypercholesteraemia. Regarding the 10-year follow-up, in those with zero CAC, the survival was 99.4%, while in those with >1000 CAC, it decreased to 87.7% (p<0.0001) (Figure 2) (12). Another cohort study of 9715 asymptomatic patients reported that the extent of CAC could accurately predict 15-year mortality in the study population (13). Based on a large prospective, population-based study of 6809 individuals between 45 and 84 years, the relationship between CAC and CAD was similar in young and elderly participants, suggesting that CAC scoring is a useful tool for risk prediction regardless of age (14).
The prospective cohort MESA (Multi-Ethnic Study of Atherosclerosis) study investigated the distribution of CAC on the basis of age, sex, ethnic background in individuals without clinically manifest cardiovascular disease. Based on their analysis of 6110 included participants, higher CAC values were measured in men, and CAC score increased with increasing age. Moreover, when studying the sex-, race and age-based differences, whites had the highest percentiles in all age group and Chinese had the lowest percentiles in the oldest age group regardless of sex. In younger participants, Hispanic women and black men had the lowest percentiles (15). This study provided the “CAC Score Reference Values” for the estimation of CAC score based on age, gender and race.
Another MESA Study of 6814 participants aimed to directly compare six risk markers including CAC, carotid intima-media thickness, ankle-brachial index, brachial flow-mediated dilatation, high-sensitivity C-reactive protein and family history of CAD (16). Their results suggest that CAC is superior in the discrimination and risk reclassification when compared with the other five markers.
In 2015 McClelland et al derived and validated a novel risk score for the estimation of 10-years CAD risk (MESA risk score) (17). Beyond traditional Framingham risk factors such as age, sex, HDL cholesterol, total cholesterol, systolic blood pressure, anti-hypertensive medication use, current smoking and diabetes, MESA risk score included CAC score, as well. External validation for testing MESA risk score was conducted in the Heinz Nixdorf Recall Study (HNR) and in the Dallas Heart Study (DHS) populations. Their results have shown that when adding CAC score to the traditional risk factors, C-statistic improved from 0.75 to 0.80 (p<0.0001). MESA risk score proved to be a very accurate tool for the estimation of 10-year CAD risk: external validation analysis resulted in 0.779 Harrell’s C-statistic in HNR and 0.816 in DHS. Until now, only MESA risk score incorporated CAC testing in the risk prediction of CAD.
The predictive value of zero CAC score
Previous studies aimed to investigate the utility of zero CAC score in the risk stratification of patients with suspected CAD (18–25). All of them concluded that zero CAC score is linked to low probability of cardiovascular events in the future.
In a study including 6814 MESA participants, zero CAC score proved to be the strongest among all negative risk markers, with an adjusted mean diagnostic likelihood ratio of 0.14±0.12 for CAD (Figure 3). Moreover, in net reclassification improvement analysis, zero CAC score resulted in the largest and most accurate downward risk reclassification (26). Another MESA study of 4758 participants, among those by whom moderate-to-high intensity statin therapy was recommended based on 2013 ACC/AHA guidelines, 41% had zero CAC and 5.2 atherosclerotic cardiovascular disease event rate of 5.2 per 1000 person-years (23). Absence of CAC was linked to extremely low CAD rate in the Population-based cohort of JUPITER (Justification for Use of Statins in Prevention: An Intervention Trial Evaluating Rosuvastatin) Study, as well (27).

Therefore, zero CAC score can help to identify those who are less likely to benefit from statin and other preventive pharmacotherapy.
The role of CAC score in primary prevention
Since CAC screening has emerged as a relatively cheap and widely accessible non-invasive imaging modality, the major guidelines and expert consensus documents have already incorporated CAC score for risk prediction and therapy guiding (Table 1).
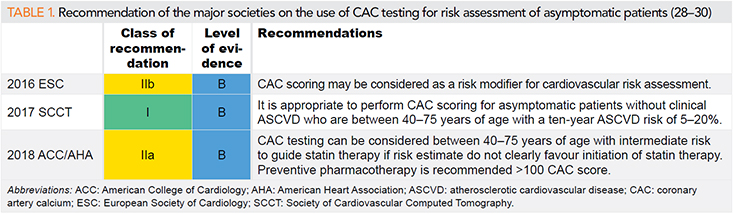
The 2016 European Society of Cardiology (ESC) guideline on cardiovascular disease prevention recommends that CAC testing may be considered as a risk modifier for cardiovascular risk assessment (28). The 2017 expert consensus of the Society of Cardiovascular Computed Tomography (SCCT) states that it is appropriate to measure CAC score for shared decision making in patients without symptoms of CAD who are between 40-75 years of age and with 5-20% ten-year risk of atherosclerotic cardiovascular disease. In those individuals with lower risk, CAC testing may be considered in selected cases, such as in those with family history of premature CAD (29). The 2018 ACC/AHA cholesterol guideline recommends that CAC scoring can be considered between 40–75 years of age with intermediate risk to guide statin therapy if risk estimate do not clearly favor initiation of statin therapy. In case of zero CAC, it is reasonable to withhold statin and initiation of preventive pharmacotherapy is recommended for those patients with >100 CAC score (30).
The difference in the recommendations of the various societies can be explained by several facts. Since the ESC guideline was published in 2016, it does not include the most recent study results, while the 2018 ACC/AHA cholesterol guideline is based on more recent data supporting the use of CAC in therapy guidance (18, 31–33). The expert consensus of the SCCT places the greatest emphasis on the role of CAC score in patient management among the three societies. However, the SCCT document is an expert consensus, which does not have the same requirements as a guideline and therefore it can be more progressive.
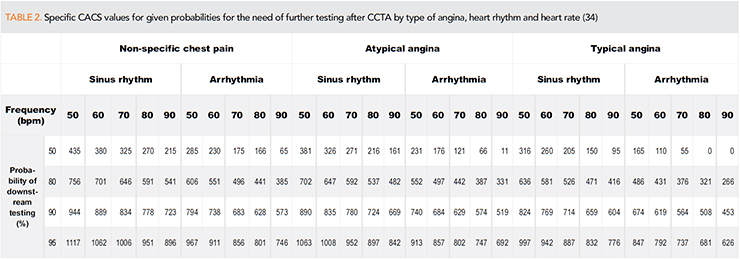
In Hungary, unfortunately, CAC scoring is not used for risk stratification in asymptomatic patients despite the strong supporting evidences. Coronary calcium scan is routinely acquired before each CCTA in symptomatic patients with suspected CAD. The non-contrast enhanced scan is used mainly for planning the CCTA image acquisition and in some cases to defer from CCTA due to very high CAC score. High CAC score values are associated not only with elevated cardiovascular risk, but they can cause artifacts resulting in non-diagnostic CCTA images. However, there are no clear-cut CAC score thresholds above which performance of CCTA is not recommended therefore it depends on the local expertise and the clinical question to decide if CCTA should be deferred. We have previously determined individualized cut-off values for given probabilities of the need of additional testing, which may facilitate personalized decision-making to perform or defer coronary CTA (Table 2) (34).
CAC screening appears to improve cooperation of asymptomatic patients (21). A meta-analysis of six studies concluded that identification of CAC was associated with significantly increased likelihood of initiating and continuing pharmacologic and lifestyle CAD prevention (35).
Limitations of CAC score-based risk prediction
Agatston score does not provide information about the total number and regional distribution of calcified plaques, which would be an important aspect of CAD risk prediction (36–38). Moreover, calcified plaques seem to be more resistant to rupture when compared with non-calcified or partially-calcified coronary artery lesions. Therefore, even if increased plaque density contributes to higher CAC score values and increased cardiovascular risk, previous studies have reported that for the same plaque volume, higher calcium density is linked to decreased risk of CAD (5, 39). Similarly, since statins can reduce the volume of non-calcified plaque components, it may lead to higher CAC score parallel with increased plaque stability (ie. paradox calcification) (40, 41).
Even if absence of CAC proved to be a strong negative marker, the CAD risk remains high in some special cases. In asymptomatic patients with zero CAC score, after adjustment for age and sex, positive family history for CAD was associated with 73% increase in CAD (42). Similarly, in those individuals with zero CAC score, mortality hazard ratio was 3.6 (95% CI: 2.3–5.7) in active smokers compared to non-smokers (43). Moreover, in MACS (Multicenter AIDS Cohort Study), HIV infection was associated with higher prevalence of non-calcified coronary artery plaque independent of other cardiovascular risk factors (44).
Conclusion
In this review we aimed to summarize the most important data on the prognostic value of CAC scoring in asymptomatic patients and its role in primary prevention. Based on the results of large population-based and cohort studies, CAC scoring is highly encouraged for further risk stratification for decision making on initiation of preventive pharmacotherapy. Moreover, CAC scoring can improve cooperation of patients and adherence to statins. For all these reasons, the major guidelines and expert consensus documents have already incorporated consideration of CAC testing into CAD risk stratification and therapy guiding. However, it is important to keep in mind, that CAC score can only identify calcified plaque components, while non-calcified coronary artery lesions cannot be excluded without CCTA. All in all, given the burden of CAD both on the patients and healthcare, utilizing CAC testing in asymptomatic patients for the purpose of primary prevention and risk stratification should be considered.
Declaration of interest
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
References
1. Knuuti J, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). European Heart Journal 2019; 41(3): 407–477. https://doi.org/10.1093/eurheartj/ehz425
2. Karanasos A LJ WK, Regar E et al. Calcified nodules: an underrated mechanism of coronary thrombosis? JACC Cardiovasc Imaging. 2012;5(10):1071-72 https://doi.org/10.1016/j.jcmg.2012.04.010.
3. Choi EK, et al. Coronary computed tomography angiography as a screening tool for the detection of occult coronary artery disease in asymptomatic individuals. J Am Coll Cardiol 2008; 52(5): 357–65.
https://doi.org/10.1016/j.jacc.2008.02.086
4. Chen J, et al. Coronary Artery Calcification and Risk of Cardiovascular Disease and Death Among Patients With Chronic Kidney Disease. JAMA Cardiol 2017; 2(6): 635–643.
https://doi.org/10.1001/jamacardio.2017.0363
5. Criqui MH, et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA 2014; 311(3): 271–8.
https://doi.org/10.1001/jama.2013.282535
6. Greenland P, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA 2004; 291(2): 210–5. https://doi.org/10.1001/jama.291.2.210
7. Mitchell JD, et al. Coronary Artery Calcium and Long-Term Risk of Death, Myocardial Infarction, and Stroke: The Walter Reed Cohort Study. JACC Cardiovasc Imaging 2018; 11(12): 1799–1806.
https://doi.org/10.1016/j.jcmg.2017.09.003
8. Paixao AR, et al. Coronary Artery Calcium Improves Risk Classification in Younger Populations. JACC Cardiovasc Imaging 2015; 8(11): 1285–93. https://doi.org/10.1016/j.jcmg.2015.06.015
9. Agatston AS, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15(4): 827–32. https://doi.org/10.1016/0735-1097(90)90282-t
10. Mao SS, et al. Comparison of coronary artery calcium scores between electron beam computed tomography and 64-multidetector computed tomographic scanner. J Comput Assist Tomogr 2009; 33(2): 175–8. https://doi.org/10.1097/RCT.0b013e31817579ee
11. McCollough CH, et al. Coronary artery calcium: a multi-institutional, multimanufacturer international standard for quantification at cardiac CT. Radiology 2007; 243(2): 527–38.
https://doi.org/10.1148/radiol.2432050808
12. Budoff MJ, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol 2007; 49(18): 1860–70. https://doi.org/10.1016/j.jacc.2006.10.079
13. Shaw LJ, et al. Long-Term Prognosis After Coronary Artery Calcification Testing in Asymptomatic Patients: A Cohort Study. Ann In