The year in cardiovascular medicine 2021: valvular heart disease
█ Current opinion
Authors:
Helmut Baumgartner1, Bernard Iung2, David Messika-Zeitoun3, Catherine M. Otto4
1Department of Cardiology III – Adult Congenital and Valvular Heart Disease, University Hospital Muenster,
Germany
2Department of Cardiology, Bichat Hospital, APHP, Université de Paris, Paris, France
3Division of Cardiology, University of Ottawa Heart Institute, Ottawa, Canada
4Division of Cardiology, Department of Medicine, University of Washington School of Medicine, Seattle, WA, USA
Received 15 September 2021; revised 15 October 2021; accepted 23 December 2021;
online publish-ahead-of-print 3 January 2022
Introduction
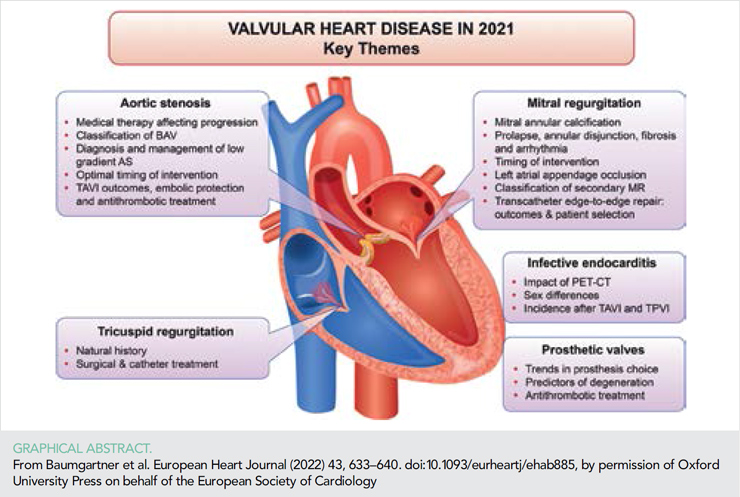
The increasing burden of valvular heart disease (VHD) – in particular in an ageing population – is recognized by medical experts, although there is less awareness of these conditions by the general public and relevant stakeholders. Together with emerging non-surgical interventional treatment options, this has led to intense research interest in VHD with an enormous number of publications during the last year. Many of these publications address interventional treatment, including technical refinements and outcomes compared with surgery or medical therapy. In addition, attention has focused on pathophysiological aspects, improved diagnosis, risk stratification, and optimal timing for intervention. Importantly, new guidelines for the management of VHD have been published by both the ESC/EACTS and ACC/AHA (1, 2). This short overview can neither address all changes in the guidelines nor acknowledge all appreciable research efforts over this year. Thus, we have selected a few papers as examples that reflect the breadth of ongoing research, with the expectation that interested readers will find additional articles using online searches.
ISSUE: CARDIOLOGIA HUNGARICA | 2022 | VOLUME 52, ISSUE 1
Aortic valve
Pathophysiology
There is increasing evidence that disease-modifying therapies for calcific aortic stenosis (AS) may be possible. Preclinical and observational studies had suggested that bone turnover and osteoblastic differentiation of valvular interstitial cells are important contributory mechanisms but in a double-blind randomized controlled trial (RCT) neither denosumab nor alendronic acid was shown to affect the progression of aortic valve calcification (3). Lee et al. (4) reported in a retrospective analysis of patients with diabetes and mild-to-moderate AS that dipeptidyl peptidase-4 inhibitors with favourable pharmacokinetic and pharmacodynamic properties were associated with lower risk of AS progression. Pérez de Isla et al. (5) reported a higher incidence of aortic valve replacement (AVR) in patients with familial hypercholesterolaemia (FH) based on data from SAFEHEART – a long-term prospective cohort study of a population with and non-affected relatives including a total of 5022 subjects. Cox regression analysis demonstrated an association between FH and AVR [hazard ratio (HR): 3.89; 95% confidence interval (CI): 1.20–12.63; P = 0.024], with older age, previous atherosclerotic cardiovascular disease, hypertension, increased LDL-cholesterol Lp(a) – years, and elevated Lp(a) being independently predictive of an event suggesting that reduction in LDL-cholesterol and Lp(a) together with control of hypertension could retard the progression of AS in FH. All these studies, however, remain only hypothesis generating, and further research is required to evaluate potential treatment options.
Diagnosis
The diagnosis of severe AS and identification of patients who benefit from intervention remains challenging in the setting of low-gradient AS. Mosleh et al. (6) reported a similar benefit of transcatheter aortic valve implantation (TAVI) in patients with high-gradient AS and paradoxical low-flow–low-gradient AS using propensity score matching. A meta-analysis including 32 studies found the similar benefit of AVR in patients with classical low-flow–low-gradient AS, paradoxical low-flow–low-gradient AS, and even normal flow–low-gradient AS (HR for all-cause mortality 0.41–0.42) (7). Conversely Freitas-Ferraz et al. (8) reported that one-third of patients with paradoxical low-flow–low-gradient AS failed to benefit from intervention. Bienjounetti-Boudreau et al. (9) reported that in patients with low-gradient AS, women had lower survival compared with men, possibly related to a lower rate of AVR, raising concerns about correct diagnosis and clinical decision-making for women in this setting. These studies emphasize the importance of an integrated approach, including additional parameters such as quantification of valve calcification, in the setting of low-gradient AS (1) to avoid both, overor undertreatment. An integrated approach also may be appropriate in patients with normal flow–low-gradient AS.
Availability of the international consensus statement on nomenclature and classification of the congenital bicuspid aortic valve and its aortopathy will be helpful for clinical, surgical, interventional, and research purposes (10).
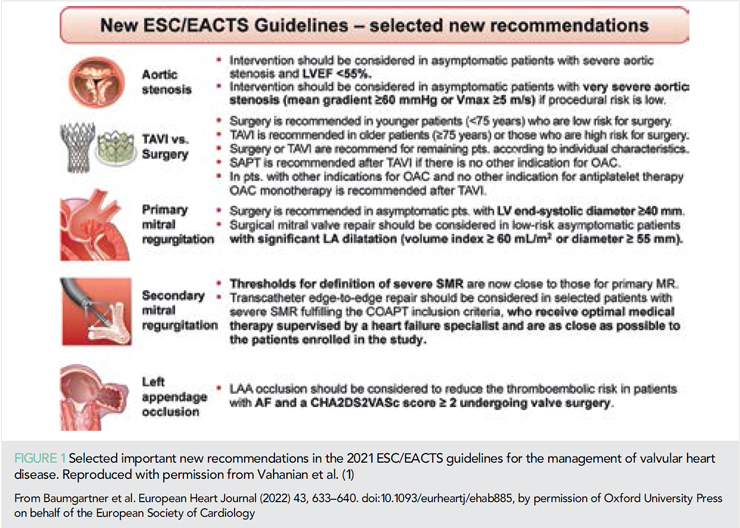
Timing of intervention
The updated ESC/EACTS and ACC/AHA guidelines continue to recommend AVR only in selected patients with asymptomatic AS although results from ongoing RCTs are awaited (1, 2). Recently, the results of the AVATAR (Aortic Valve ReplAcemenT versus conservative treatment in Asymptomatic seveRe aortic stenosis) Trial were published (11). In 157 patients with severe asymptomatic AS (including a negative exercise test) who were randomly allocated to early surgery or conservative treatment, the surgical group had a significantly lower incidence of the primary composite endpoint (all-cause mortality, acute myocardial infarction, stroke or unplanned hospitalization for heart failure). These findings require confirmation in larger studies and over a longer follow-up time, given the use of a combined endpoint and the issue of valve durability over the patient’s lifetime. In the current guidelines, the thresholds where intervention should be considered (Class IIa recommendation) in asymptomatic patients with severe AS were lowered to left ventricular ejection fraction (LVEF) < 55% and peak transvalvular velocity ≥5 m/s in surgical low-risk patients (1) (Figure 1).
Jean et al. (12) reported that in a series of patients with heart failure (HF) and reduced ejection fraction, moderate AS was associated with a marked incremental risk of mortality. Aortic valve replacement, and especially TAVI during follow-up, was associated with improved survival supporting the realization of RCTs to assess the effect of early transcatheter AVR in these patients.
Patients with established indication for AVR require timely treatment. This was once more emphasized by a study reporting significant mortality on the waiting list for surgical as well transcatheter AVR (13).
Type of intervention
The choice between TAVI and surgical AVR (SAVR) remains a matter of controversy in patients suitable for both interventions. In a meta-analysis of currently available RCTs, Zhang et al. (14) raise concerns regarding the long-term outcome of TAVI. While 2-year results for all-cause mortality, the combined endpoint of all-cause mortality and stroke, and cardiovascular mortality were similar for the two modalities, 2 to 5-year results favoured surgery. Possible explanations for this observation include higher rates of more than mild paravalvular regurgitation and conduction disturbances (pacemaker requirement, left bundle branch block) after TAVI which may affect long-term, but not short-term, outcomes. The 2-year analysis of PARTNER 3 (balloon-expandable TAVI vs. SAVR in low-risk patients) found a decreasing but still significant difference in favour of TAVI for the composite of death, stroke, and rehospitalization for HF but no longer a significant difference for death or stroke alone (15). The 8-year results of the NOTION trial (16) – so far the longest follow-up for an RCT with the majority of patients included being at low surgical risk – continue to show no difference in all-cause mortality (Figure 2) or the composite of all-cause mortality, stroke, and myocardial infarction.
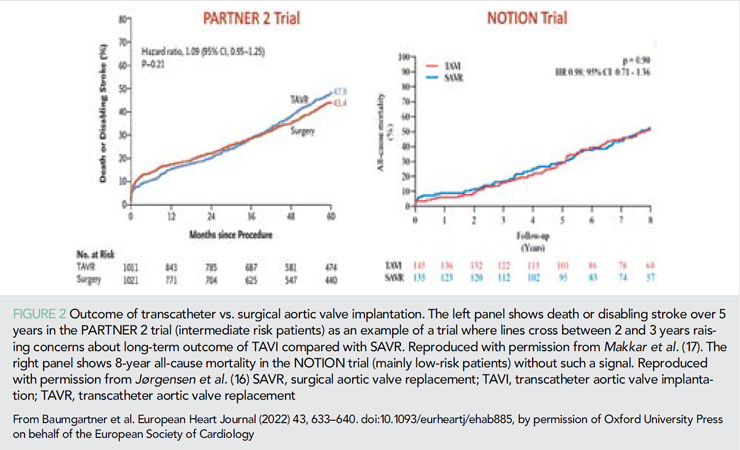
Haemodynamic results were slightly but still significantly better for TAVI with a lower rate of structural valve deterioration although the latter was driven by the higher residual gradients in the surgical group. For the more clinically relevant endpoint of prosthetic valve failure (valve-related death, severe structural valve deterioration, or valve re-intervention), there was no difference between study groups. This trial supports non-inferiority of TAVI in the long-term but has several limitations (small patient numbers, incomplete echo data and no core lab, and a significant proportion of surgical valve types with known suboptimal results). Therefore, long-term data still need to be collected carefully and the extension of TAVI to younger low-risk patients must be considered with caution. In addition to higher rates of paravalvular regurgitation and conduction disturbances the issue of valve durability, which appears to be valve specific, remains a concern. For the balloon-expandable Edwards valve, the performance of the second generation was worse than for the surgical valve while the third generation was non-inferior (18).
Potentially limited access to the coronary arteries after TAVI also remains a matter of concern. Although high success rates for the cannulation of coronaries have been reported, in particular for short stent-frame prosthesis, failure of percutaneous coronary intervention (PCI) was close to 10%19,20 and must be expected to markedly increase after redo-TAVI.21 Patients with ST-elevation myocardial infarction after TAVI had a significantly longer door-to-balloon time and a four-fold higher PCI failure rate associated with poor outcome compared with patients without TAVI (22).
Current ACC/AHA guidelines opened the range where individual shared decision-making (heart team and patient weigh individual advantages and disadvantages of TAVI and SAVR) to patients between age 65 and 80 years or life expectancy 10–20 years, respectively (2). The ESC/EACTS guidelines remained more conservative recommending SAVR for all low-risk patients younger than 75 years (IB) and TAVI for patients 75 years and older or patients at high surgical risk (IA) while leaving the remaining patients for individual decision (1).
Complications after transcatheter aortic valve implantation
Although the stroke rate has become relatively low after TAVI, it remains one of the most devastating complications and embolic protection devices that may potentially further reduce this risk are intensively investigated. In a meta-analysis, more than 70% of patients had evidence of silent brain injury after TAVI which was associated with increased incidence of early cognitive dysfunction but still unclear long-term effects (23). Cerebral embolic protection devices reduced the volume but did, however, not affect the incidence and the number of injuries per patient. Several other studies could so far not demonstrate a reduction in clinical event rates with the use of protection devices (24–26).
After TAVI, the current recommendation is to use single platelet therapy in patients without other indication for oral anticoagulation or dual antiplatelet therapy, and to use oral anticoagulation only in those with established indication and no other indication for antiplatelet therapy, based on results from several RCTs (27). Non-vitamin K antagonist oral anticoagulants (NOACs) may be a good alternative to warfarin when oral anticoagulation is indicated (28, 29) – although a recent RCT reported a higher bleeding rate (30). One study reported that clopidogrel may be superior to aspirin for single antiplatelet therapy (31). In another RCT of low-risk patients, warfarin was associated with less subclinical valve thrombosis without increased bleeding risk (32). However, considering the still unclear impact of subclinical valve thrombosis, the use of routine anticoagulation remains questionable even in these patients.
Significant residual mitral regurgitation (MR) after TAVI has been shown once more to have negative impact on outcome (33) and percutaneous mitral valve repair may then improve symptoms and outcome (34), but further prospective studies will be required to prove this concept.
Mitral valve disease
Calcific mitral valve disease
Calcific mitral valve disease (CMVD) is due to mitral annular calcification (MAC) that extends into the leaflets and can present as mitral stenosis (MS), MR, or a combination of both. Patients with CMVD are mostly elderly, with a strong female predominance and multiple comorbidities (35). They are often left untreated even when symptomatic and experienced a poor outcome predicted by severity of the disease (valve area/gradient) and pulmonary artery pressure. The independent prognostic value of the transmitral gradient – irrespective of MR degree – was confirmed in a second study (36). Transmitral gradient is easy to measure but is dependent on haemodynamic conditions (stroke volume and heart rate). The projected gradient, adjusting for these two parameters, improved diagnostic concordance for MS severity and thresholds of 4 and 6 mmHg for moderate and severe MS provided a better risk stratification than the commonly used thresholds of 5 and 10 mmHg (37). Surgery is high risk, and transcatheter mitral valve interventions have emerged as an alternative but remain associated with high mortality and expose to left ventricular outflow tract (LVOT) obstruction and paravalvular regurgitation (38). Acceptable procedural and clinical outcomes could be achieved using pre-emptive strategies (alcohol septal ablation) as in the MITRAL prospective registry, but two-thirds of patients had to be excluded because of high risk of LVOT obstruction, prosthesis embolization, or both (39).
Mitral valve prolapse, mitral annular disjunction, fibrosis, and arrhythmia
In 400 patients with mitral valve prolapse (MVP) enrolled in two centres, myocardial replacement fibrosis – late gadolinium enhancement (LGE) assessed using cardiac magnetic resonance imaging (CMR) – was common (prevalence 28%), preferentially located in the basal infero-lateral wall and papillary muscle, was associated with MR severity, left ventricular (LV) remodelling (LV volume and mass), ventricular arrhythmia, and with an increased risk of cardiovascular events (incremental to echocardiographic information) (40). Interestingly, the relationship between LGE and ventricular arrhythmia was more pronounced in patients with no/mild or moderate MR than in patients with severe MR favouring the pathophysiologic hypothesis that abnormalities of the mitral valve apparatus lead to fibrosis responsible for ventricular arrhythmia rather than a causal role of MR. An association between mitral annular disjunction (MAD), leaflet redundancy or bileaflet MVP/Barlow disease, and ventricular arrhythmia has been reported (41, 42) and mortality rate increased with ventricular arrhythmia grade especially under conservative management (41). However, the relationship between MAD and mortality remained unclear (43). When assessed in patients with structurally normal heart who underwent a CT scan, the prevalence of MAD was reported to be very high (96%) (44). In addition, the prevalence of MAD widely varied according to the imaging technique. Transthoracic echocardiography (TTE) exhibited a good specificity but a low sensitivity compared with MRI or transoesophageal echocardiography (TEE) (45). Large prospective studies are strongly needed to standardize the definition and methodology of MAD measurement and to better define the arrhythmogenic risk of MVP and MAD as well as the potential role of LGE to guide indications for surgery in patients with severe primary MR.
Timing of intervention
In asymptomatic patients with primary MR, both the ESC/EACTS and ACC/AHA guidelines now recommend surgery when LV end-systolic diameter reaches 40 mm (previously 45 mm) (1). The ESC/EACTS guidelines also emphasize the importance of left atrium enlargement (≥60 mL/m2 or ≥55 mm) in asymptomatic patients in sinus rhythm with preserved EF and LV end-systolic diameter <40 mm if surgical risk if low and likelihood of repair high when surgery is performed in a Heart Valve Centre (Class IIa recommendation). The ACC/AHA guidelines consider valve repair reasonable in asymptomatic patients with severe MR, normal LV size and function, low surgical risk and a repairable valve, regardless of the left atrial size.
Anticoagulation and stroke
The Left Atrial Appendage Occlusion during Cardiac Surgery to Prevent Stroke (LAOOS III) trial has evaluated the efficacy and safety of concomitant left atrial appendage (LAA) occlusion (vs. no occlusion) in patients in atrial fibrillation and a CHAD2DS2-Vasc score ≥2 undergoing cardiac surgery, of whom 36% had a mitral valve procedure (46). The trial showed a reduction of the risk of stroke or systemic embolic event [4.8 vs. 7.0%, HR = 0.67 (0.53–0.85), P = 0.0010] in those with LAA occlusion. The data support current ACC/AHA and ESC guidelines that LAA ligation or excision along with surgical pulmonary vein isolation or a maze procedure, are reasonable in patients with VHD and AF who are undergoing surgical intervention.
Secondary mitral regurgitation – thresholds and prognostic impact
Multiple recent studies have confirmed the association between secondary mitral regurgitation (SMR) and adverse outcome even with only mild MR (47–49). However, the new ESC/EACTS guidelines have adopted the definition for severe SMR (as ACC/AHA guidelines have done before) of an effective regurgitant orifice ≥40 mm2 or regurgitant volume ≥60 mL acknowledging that a lower threshold (effective regurgitant orifice ≥30 mm2 or regurgitant volume ≥45 mL) may be applied, especially if the effective regurgitant orifice is elliptical or in low-flow conditions. The main reason supporting this change is the lack of evidence that surgical or transcatheter treatment improved outcome in patients with lower effective regurgitant orifice or regurgitant volume (i.e. moderate MR) (50, 51)
Transcatheter mitral valve interventions
In the COAPT trial, patients randomized to mitral transcatheter edge-to-edge repair (TEER) continued to show a higher event-free survival, lower mortality, and higher functional improvement compared with guideline-directed medical therapy, with a sustained reduction in MR severity through 3 years (Figure 3). Important prognostic factors identified in the COAPT population include pulmonary hypertension, tricuspid regurgitation (TR) severity, NYHA functional class, Kansas City Cardiomyopathy Questionnaire score, and 6 min walk distance (53–57). The importance of these parameters and of right ventricular dysfunction have also been reported in observational studies (58). However, mitral TEER still was beneficial, even in patients with poor prognostic factors, as long as a significant reduction in MR severity was achieved. It is worth noting that non-ambulatory patients, as those with severe pulmonary hypertension or moderate/severe right ventricular dysfunction were excluded from the COAPT study (59).
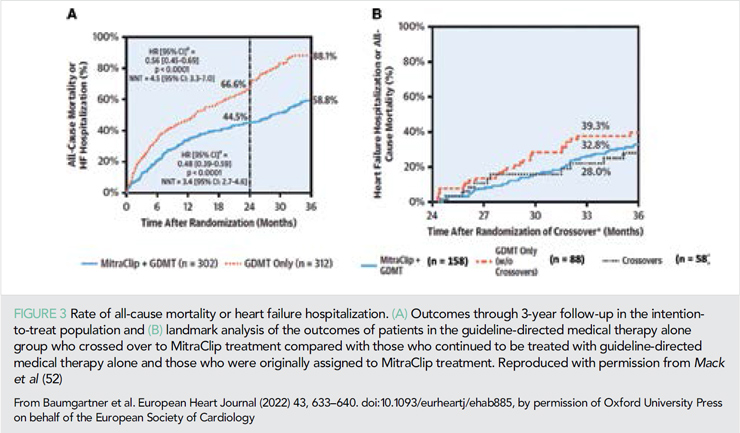
The concept of proportionate/disproportionate MR has been proposed as a framework to reconcile the discordant results of the COAPT and MITRA-FR studies. In a sub-analysis of COAPT, a small subgroup of COAPT patients – resembling those patients enrolled in MITRA-FR did indeed not achieve improvement in all-cause mortality or HF admissions at 24 months. However, they still had a significant benefit on patient-centred outcomes (60). On the other side, no benefit of the intervention was observed in MITRA-FR subgroups of patients with the so-called disproportionate MR or ‘COAPT-eligible patients’ (61, 62).
In a sub-analysis of COAPT, reduced MR at 30 days was associated with improved outcome through 2-year follow-up regardless whether the MR reduction was achieved by TEER or medical therapy. Surprisingly, one-third in the latter group had grade +2 or less at 30 days (63). Observational studies have confirmed the prognostic impact of residual MR severity (as well as of durable MR reduction) (64, 65), especially in patients with less advanced disease (LV dilatation/RV dysfunction) suggesting that in those with advanced disease the benefit of the intervention remains uncertain (66).
Although the reasons for the discrepant results between the two RCTs are still not fully understood, the recently released ESC/EACTS and ACC/AHA guidelines recommend TEER with a Class IIa, in the absence of the need for concomitant surgery, in selected patients with severe SMR fulfilling the COAPT inclusion criteria, who receive optimal medical therapy supervised by an HF specialist and are as close as possible to the patients actually enrolled in the study (1, 2).
With the increasing number of TEER performed worldwide, the management and outcomes of patients with failed TEER (up to 30% in real-life) is of utmost interest. In the STS database, 463 patients with failed TEER who underwent a non-urgent cardiac surgery were identified between 2014 and 2020 (67). Thirty-day mortality was 10.6% and repair rate only 5%. Even if most patients with failed TEER are likely conservatively managed, these data are critical as TEER indications are extending to lower risk and younger patients.
The Valve In Valve International Data Registry (VIVID) reported the mid-term clinical, haemodynamic, and echocardiographic outcome of mitral valve in valve (ViV) (N = 857) and valve in ring (ViR) (N = 222) performed between 2006 and 2020 across 90 centres worldwide.68 This registry showed that residual MS and regurgitation were common and associated with worse outcome. Immediate complications and mid-term survival were markedly worse in ViR than in ViV. The STS/ACC transcatheter valve therapy reported immediate and 1-year results of ViV implantation with the Sapien 3® in a cohort of 1529 patients (69). Most patients experienced significant and sustained functional improvement but as noted in the VIVID registry, the mean gradient was in average 7 mmHg. Transeptal access was associated with a lower 1-year mortality rate than transapical access (16 vs. 22%, P = 0.03).
A word of caution
There are concerns about potential oesophageal injury due to the duration of TEE imaging needed to guide complex transcatheter procedures. A systematic upper endoscopy was performed before and after intervention in 50 patients (mainly TEER and LAA occlusion) showing a high rate of new oesophageal injury (86%), often complex (haematoma and mucosal laceration) predicted by longer procedural time, suboptimal image quality, and pre-existing oesophageal lesions (70). With the growing number of interventions requiring TEE guidance in an ageing population with frequent comorbidities, frequent use of anticoagulant or antiplatelet agents, this study shows the need to develop alternative approaches and preventive measures to minimize gastro-intestinal complications.
Tricuspid valve disease
Tricuspid regurgitant severity and clinical outcomes
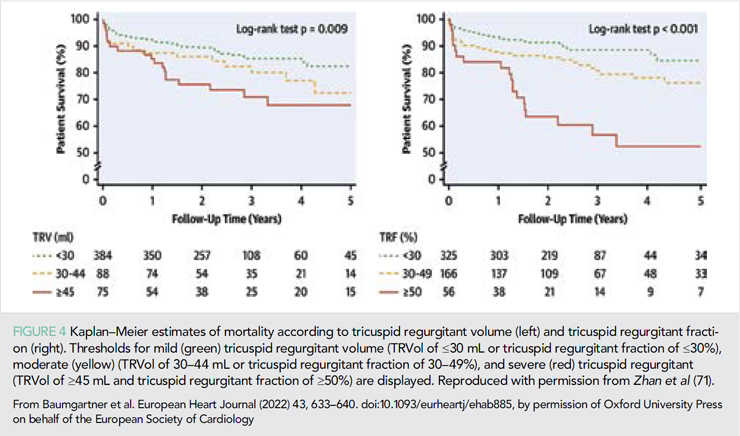
There is ample evidence that more severe TR is associated with a higher risk of adverse cardiovascular outcomes as exemplified in several studies over the last year. For example, in a single US centre registry of patients undergoing CMR over a 10-year time span, Zhan et al. (71) identified 547 patients (mean age 60 years, 53% male) with secondary (functional) TR, after excluding those with atrial fibrillation, primary tricuspid valve (TV) disease, confounding causes of right ventricular remodeling, implanted cardiac electronic devices, and medical conditions with competing risk such as heart transplantation or metastatic cancer (71). In these 547 patients, a regurgitant volume ≥45 mL or a regurgitant fraction ≥50% identified a high-risk subgroup (Figure 4) with each 10 mL increase in TR regurgitant volume associated with an adjusted HR of 1.15 (95% CI: 1.04–1.26) for death based on multivariable analysis that included clinical and biventricular imaging parameters.
Surgical management for tricuspid regurgitant is not ideal
Clinical outcomes with isolated TV surgery are poor. In a multicentre French administrative database of 5661 patients who underwent TV surgery over a 10 year period, 466 (8%) were an isolated TV procedure (repair in 41%, bioprosthetic valve in 57%, and mechanical valve in 2%) (72). About one-half patients had secondary vs. primary TR (most often due to endocarditis) with higher in-hospital mortality (14 vs. 6%) and lower 5-year survival rates free of HF readmission (62% vs. 75%), but the main determinant of outcome was the clinical presentation and not the aetiology/mechanism.
The effect of concomitant TV repair during mitral valve surgery for degenerative MR in patients with moderate TR or less-than-moderate TR but with annular dilation was studied in a recent RCT (73). Patients with TV repair had a lower incidence of a primary-endpoint event (reoperation for TR, progression of TR by two grades or severe TR, or death) at 2 years. The reduction was driven by less frequent progression of TR. These findings demonstrate the efficacy of TV repair in the reduction of TR over time. However, long-term follow-up based on clinical endpoints is needed to determine if clinical benefit of TR reduction outweighs the almost six-fold higher risk of needing a permanent pacemaker.
Transcatheter interventions
Several types of transcatheter devices can be used to reduce the severity of TR with an acceptable low rate of immediate and mid-term complications (74). However, it remains challenging to select patients most likely to benefit from these procedures. Although echocardiography remains the primary modality for identifying patients with severe TR and evaluating whether anatomy is amenable to a transcatheter repair procedure, more recent data suggest that haemodynamic parameters provide additional information in patient selection. In an international multicentre study of 236 patients undergoing transcatheter tricuspid repair, 1-year survival was only 38% in those with pre-capillary dominant pulmonary hypertension compared with 92% in those without pulmonary hypertension and 78% in those with post-capillary pulmonary hypertension (75).
Need for randomized controlled trials
Although there is ample evidence that more severe TR is associated with a higher risk of adverse outcome, there is less evidence that interventions to reduce TR severity prevent those adverse outcomes. Is TR simply a marker of increased risk or is there direct cause–effect relationship between TR severity and outcome that is independent of associated disease such as mitral valve disease, pulmonary hypertension, arrhythmias, and right ventricular dysfunction? Randomized controlled trials of TV surgery and transcatheter intervention, compared with optimal medical therapy and to each other, are needed.
Infective endocarditis
Diagnosis of prosthetic infective endocarditis (IE) is improved with 18 fluorine-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG-PET/CT) imaging. In a prospective multicentre study designed for assessing the diagnostic and therapeutic impact of 18F-FDG-PET/CT, diagnostic classification was upgraded in 24% of patients with prosthetic IE and 6% with native IE (76). Therapeutic management was changed in 21 and 31% of patients, respectively. Despite less frequent cardiac uptake, extra-cardiac uptake has an impact on the management of patients with native IE.
In a multicentre cohort of 3451 patients with IE, women were older and had more frequent staphylococcal IE than men (77). Surgery was less frequently performed in women (38 vs. 50%), including in propensity-matched cohorts. In-hospital mortality was higher in women (33% vs. 26%), as was age-adjusted mortality (odds ratio: 1.25, 95% CI: 1.07–1.47). These findings draw attention on possible sex-related differences in the management of IE.
Among 134 717 TAVI procedures in Medicare patients with 1868 cases of IE, the annual incidence of IE was 0.87% (78). Mortality was 46% at 1 year and was increased three-fold in adjusted analysis. Stroke complicated 10% of IE after TAVI and was associated with a strong increase in 1-year mortality (79).
A multicentre registry totalling 2476 patients who underwent transcatheter pulmonary valve replacement confirmed that IE was frequent, with an annual incidence of 2.2% (80). Younger age prior IE, and high gradient, but not the type of prosthesis increased the risk of IE.
Prosthetic valves
In an analysis of 253 100 AVR and 284 962 mitral valve replacements performed in the USA between 2008 and 2017, the percentage of mechanical prosthesis decreased from 45 to 17% in aortic position and from 60 to 29% in mitral position (81). Decreased use of mechanical prostheses was observed in all age groups and was more pronounced after the mid-2010s, which may reflect changes in guidelines (2) and the growing availability of transcatheter ViV procedures. The contra-indication of NOACs for mechanical prosthesis is based on a single small Phase II study using a factor IIa-inhibitor. A randomized trial comparing a Xa-inhibitor with warfarin in aortic prostheses is thus needed and might have an impact on practices (82).
The quantification of aortic bioprosthetic leaflet calcification using CT predicts subsequent bioprosthesis degeneration and clinical events, as assessed in a series of 204 patients evaluated a median of 7 years after SAVR (83). The quantification of bioprosthetic calcification may help identify patients at high risk of valve degeneration and serve as a surrogate endpoint for future studies. 18F-sodium fluoride (18F-NaF) is a marker of valve calcification activity and of early bioprosthetic leaflet degeneration. In a prospective study on 47 patients treated by TAVI and 51 patients treated by SAVR, 18F-NaF PET/CT uptake was an independent predictive factor of subsequent degeneration of transcatheter and surgically implanted aortic bioprostheses (84). There was no difference in the magnitude of degeneration between TAVI vs. surgical valves. Interestingly, this study also showed ongoing calcification activity in the native aortic valve outside the TAVI prosthesis.
Antithrombotic therapy after bioprosthetic AVR remains debated and recommendations on early anticoagulation have been upgraded (1, 2). In a nationwide analysis of 9539 patients, exposure to warfarin was associated with a lower incidence of ischaemic stroke (HR: 0.49; 95% CI: 0.35–0.70) and any thromboembolism than single antiplatelet therapy, at the expense of an increased risk of haemorrhagic stroke (HR: 1.94; 95% CI: 1.07–3.51) and major bleeding (85). Difficulties in the analysis of risk–benefit analysis highlight the need for randomized trials.
The randomized trial RIVER filled an important gap is the use of NOACs in patients with a mitral bioprosthesis and in atrial fibrillation since patients with bioprosthesis were excluded or under-represented in previous trials (86). In 1005 patients, rivaroxaban was non-inferior to warfarin for a primary composite endpoint of death, major cardiovascular events, or major bleeding at 1 year (Figure 1). NOACs can now be recommended with higher levels of evidence in patients with a bioprosthesis (1).
Outlook
This year brought important new insights in pathophysiology, diagnosis, and treatment of VHD but left and raised important questions to be addressed in the future. Fortunately, there are several ongoing trials which already work on this. Better understanding of the development of VHD and how to interfere with its progression remains a critical issue. Correct diagnosis, proper selection of patients who benefit from intervention and appropriate timing remain important issues in general and in particular in secondary mitral and TR. Emerging catheter interventional treatment options require further evaluation of efficacy, safety, and outcome compared with surgical treatment or optimal medical treatment. The field of research is definitely expanding, and progress based on ongoing research expected.
Conflict of interest: H.B.: speaker fees and congress travel support from Edwards Lifesciences and Actelion. C.M.O. and B.I.: nothing to declare. D.M.-Z.: research grant from Edwards Lifesciences.
The mention of trade names, commercial products organizations, and the inclusion of advertisements in the journal does not imply endorsement by the European Heart Journal, the editors, the editorial board, Oxford University Press or the organization to which the authors are affiliated. The editors and publishers have taken all reasonable precautions to verity drug names and doses, the results of experimental work and clinical findings published in the journal. The ultimate responsibility for the use and dosage of drugs mentioned in the journal and in interpretation of published material lies with the medical practitioner, and the editors and publisher cannot accept liability for damages arising from any error or omissions in the journal. Please inform the editors of any errors.
The opinions expressed in the European Heart Journal are those of the authors and contributors, and do not necessarily reflect those of the European Society of Cardiology, the editors, the editorial board, Oxford University Press or the organization to which the authors are affiliated.Published on behalf of the European Society of Cardiology. © The Author(s) 2020.
For Permissions, please e-mail: journals.permissions@oup.com
All rights reserved; no part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise without the prior written permission of the Publishers.
REFERENCES
1. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 2021: ehab395.
2. Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart dis ease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2020; 143: e72–e227.
3. Pawade TA, Doris MK, Bing R, et al. Effect of denosumab or alendronic acid on the progression of aortic stenosis: a double-blind randomized controlled trial. Circulation 2021; 143: 2418–2427.
4. Lee S, Lee S-A, Choi B, et al. Dipeptidyl peptidase-4 inhibition to prevent progression of calcific aortic stenosis. Heart 2020; 106: 1824–1831.
5. Pérez de Isla L, Watts GF, Alonso R, et al. Lipoprotein(a), LDL-cholesterol, and hypertension: predictors of the need for aortic valve replacement in familial hypercholesterolaemia. Eur Heart J 2021; 42: 2201–2211.
6. Mosleh W, Amer MR, Ding Y, et al. Benefit of transcatheter aortic valve replacement in patients with paradoxical low-flow low gradient versus high-gradient aortic stenosis and preserved left ventricular function. Circ Cardiovasc Interv 2021; 14: e010042.
7. Ueyama H, Kuno T, Harrington M, et al. Impact of surgical and transcatheter aortic valve replacement in low-gradient aortic stenosis: a meta-analysis. JACC Cardiovasc Interv 2021; 14: 1481–1492.
8. Freitas-Ferraz AB, Nombela-Franco L, et al. Transcatheter aortic valve replacement in patients with paradoxical low-flow, low-gradient aortic stenosis: incidence and predictors of treatment futility. Int J Cardiol 2020; 316: 57–63.
9. Bienjonetti-Boudreau D, Fleury M-A, Voisine M, et al. Impact of sex on the management and outcome of aortic stenosis patients. Eur Heart J 2021; 42: 2683–2691.
10. Michelena HI, Della Corte A, Evangelista A, et al. International consensus statement on nomenclature and classification of the congenital bicuspid aortic valve and its aortopathy, for clinical, surgical, interventional and research purposes. Eur J Cardiothorac Surg 2021; 60: 448–476.
11. Banovic M, Putnik S, Penicka M, et al. Aortic valve ReplAcemenT versus conservative treatment in asymptomatic SeveRe aortic stenosis: the AVATAR trial. Circulation; https://doi.org/10.1161/CIRCULATIONAHA.121.057639. Published online ahead of print 13 November 2021.
12. Jean G, Van Mieghem NM, Gegenava T, al. Moderate aortic stenosis in patients with heart failure and reduced ejection fraction. J Am Coll Cardiol 2021; 77: 2796–2803.
13. Albassam O, Henning KA, Qiu F, et al. Increasing wait-time mortality for severe aortic stenosis: a population-level study of the transition in practice from surgical aortic valve replacement to transcatheter aortic valve replacement. Circ Cardiovasc Interv 2020; 13: e009297.
14. Zhang X-L, Zhang X-W, Lan R-F, et al. Long-term and temporal outcomes of transcatheter versus surgical aortic-valve replacement in severe aortic stenosis: a meta-analysis. Ann Surg 2021; 273: 459–466.
15. Leon MB, Mack MJ, Hahn RT, et al. Outcomes 2 years after transcatheter aortic valve replacement in patients at low surgical risk. J Am Coll Cardiol 2021; 77: 1149–1161.
16. Jørgensen TH, Thyregod HGH, Ihlemann N, et al. Eight-year outcomes for patients with aortic valve stenosis at low surgical risk randomized to transcatheter vs. surgical aortic valve replacement. Eur Heart J 2021; 42: 2912–2919.
17. Makkar RR, Thourani VH, Mack MJ, et al. Five-year outcomes of transcatheter or surgical aortic-valve replacement. N Engl J Med 2020; 382: 799–809.
18. Pibarot P, Ternacle J, Jaber WA, et al. Structural deterioration of transcatheter versus surgical aortic valve bioprostheses in the PARTNER-2 trial. J Am Coll Cardiol 2020; 76: 1830–1843.
19. Barbanti M, Costa G, Picci A, et al. Coronary cannulation after transcatheter aortic valve replacement: the RE-ACCESS study. JACC Cardiovasc Interv 2020; 13: 2542–2555.
20. Kim WK, Pellegrini C, Ludwig S, et al. Feasibility of coronary access in patients with acute coronary syndrome and previous TAVR. JACC Cardiovasc Interv 2021; 14: 1578–1590.
21. Buzzatti N, Montorfano M, Romano V, et al. A computed tomography study of coronary access and coronary obstruction after redo transcatheter aortic valve implantation. EuroIntervention 2020; 16: e1005–e1013.
22. Faroux L, Lhermusier T, Vincent F, et al. ST-segment elevation myocardial infarction following transcatheter aortic valve replacement. J Am Coll Cardiol 2021; 77: 2187–2199.
23. Woldendorp K, Indja B, Bannon PG, et al. Silent brain infarcts and early cognitive outcomes after transcatheter aortic valve implantation: a systematic review and meta-analysis. Eur Heart J 2021; 42: 1004–1015.
24. Butala NM, Makkar R, Secemsky EA, et al. Cerebral embolic protection and outcomes of transcatheter aortic valve replacement: results from the transcatheter valve therapy registry. Circulation 2021; 143: 2229–2240.
25. Lansky AJ, Makkar R, Nazif T, et al. A randomized evaluation of the TriGuard™ HDH cerebral embolic protection device to Reduce the Impact of Cerebral Embolic LEsions after TransCatheter Aortic Valve ImplanTation: the REFLECT I trial. Eur Heart J 2021; 42: 2670–2679.
26. Stachon P, Kaier K, Heidt T, et al. The use and outcomes of cerebral protection devices for patients undergoing transfemoral transcatheter aortic valve replacement in clinical practice. JACC Cardiovasc Interv 2021; 14: 161–168.
27. Ten Berg J, Sibbing D, Rocca B, et al. Management of antithrombotic therapy in patients undergoing transcatheter aortic valve implantation: a consensus document of the ESC Working Group on Thrombosis and the European Association of Percutaneous Cardiovascular Interventions (EAPCI), in collaboration with the ESC Council on Valvular Heart Disease. Eur Heart J 2021; 42: 2265–2269.
28. Didier R, Lhermusier T, Auffret V, et al. TAVR patients requiring anticoagulation: direct oral anticoagulant or vitamin K antagonist? JACC Cardiovasc Interv 2021; 14: 1704–1713.
29. Kawashima H, Watanabe Y, Hioki H, et al. Direct oral anticoagulants versus vitamin k antagonists in patients with atrial fibrillation after TAVR. JACC Cardiovasc Interv 2020; 13: 2587–2597.
30. Van Mieghem NM, Unverdorben M, Hengstenberg C, et al. Edoxaban versus vitamin K antagonist for atrial fibrillation after TAVR. N Engl J Med 2021; 385: 2150–2160.
31. Kobari Y, Inohara T, Saito T, et al. Aspirin versus clopidogrel as single antithrombotic therapy after transcatheter aortic valve replacement: insight from the OCEAN-TAVI registry. Circ Cardiovasc Interv 2021; 14: e010097.
32. Rogers T, Shults C, Torguson R, et al. Randomized trial of aspirin versus warfarin after transcatheter aortic valve replacement in low-risk patients. Circ Cardiovasc Interv 2021; 14: e009983.
33. Witberg G, Codner P, Landes U, et al. Effect of transcatheter aortic valve replacement on concomitant mitral regurgitation and its impact on mortality. JACC Cardiovasc Interv 2021; 14: 1181–1192.
34. Witberg G, Codner P, Landes U, et al. Transcatheter treatment of residual significant mitral regurgitation following TAVR: a multicenter registry. JACC Cardiovasc Interv 2020; 13: 2782–2791.
35. Kato N, Padang R, Scott CG, et al. The natural history of severe calcific mitral stenosis. J Am Coll Cardiol 2020; 75: 3048–3057.
36. Bertrand PB, Churchill TW, Yucel E, Namasivayam M, Bernard S, Nagata Y, et al. Prognostic importance of the transmitral pressure gradient in mitral annular calcification with associated mitral valve dysfunction. Eur Heart J 2020; 41: 4321–4328.
37. Kato N, Pislaru SV, Padang R, et al. A novel assessment using projected transmitral gradient improves diagnostic yield of Doppler hemodynamics in rheumatic and calcific mitral stenosis. JACC Cardiovasc Imaging 2021; 14: 559–570.
38. Urena M, Vahanian A, Brochet E, et al. Current indications for transcatheter mitral valve replacement using transcatheter aortic valves: valve-in-valve, valve-in-ring, and valve-in-mitral annulus calcification. Circulation 2021; 143: 178–196.
39. Guerrero M, Wang DD, Eleid MF, et al. Prospective study of TMVR using balloon-expandable aortic transcatheter valves in MAC: MITRAL trial 1-year outcomes. JACC Cardiovasc Interv 2021; 14: 830–845.
40. Constant Dit Beaufils A-L, Huttin O, Jobbe-Duval A, et al. Replacement myocardial fibrosis in patients with mitral valve prolapse: relation to mitral regurgitation, ventricular remodeling, and arrhythmia. Circulation 2021; 143: 1763–1774.
41. Essayagh B, Sabbag A, Antoine C, et al. Presentation and outcome of arrhythmic mitral valve prolapse. J Am Coll Cardiol 2020; 76: 637–649.
42. van Wijngaarden AL, de Riva M, Hiemstra YL, et al. Parameters associated with ventricular arrhythmias in mitral valve prolapse with significant regurgitation. Heart 2021; 107: 411–418.
43. Essayagh B, Sabbag A, Antoine C, et al. The mitral annular disjunction of mitral valve prolapse: presentation and outcome. JACC Cardiovasc Imaging 2021; 14: 2073–2087.
44. Toh H, Mori S, Izawa Y, et al. Prevalence and extent of mitral annular disjunction in structurally normal hearts: comprehensive 3D analysis using cardiac computed tomography. Eur Heart J Cardiovasc Imaging 2021; 22: 614–622.
45. Mantegazza V, Volpato V, Gripari P, et al. Multimodality imaging assessment of mitral annular disjunction in mitral valve prolapse. Heart 2021; 107: 25–32.
46. Whitlock RP, Belley-Cote EP, Paparella D, et al. Left atrial appendage occlusion during cardiac surgery to prevent stroke. N Engl J Med 2021; 384: 2081–2091.
47. Bartko PE, Heitzinger G, Pavo N, et al. Burden, treatment use, and outcome of secondary mitral regurgitation across the spectrum of heart failure: observational cohort study. BMJ 2021; 373: n1421.
48. Benfari G, Antoine C, Essayagh B, et al. Functional mitral regurgitation outcome and grading in heart failure with reduced ejection fraction. JACC Cardiovasc Imaging 2021; 14: 2303–2315.
49. Pagnesi M, Adamo M, Sama IE, et al. Impact of mitral regurgitation in patients with worsening heart failure: insights from BIOSTAT-CHF. Eur J Heart Fail 2021; 23: 1750–1758.
50. Michler RE, Smith PK, Parides MK, Ailawadi G, Thourani V, Moskowitz AJ, et al. Two-year outcomes of surgical treatment of moderate ischemic mitral regurgita- tion. N Engl J Med 2016; 374: 1932–1941.
51. Obadia J-F, Messika-Zeitoun D, Leurent G, et al. Percutaneous repair or medical treatment for secondary mitral regurgitation. N Engl J Med 2018; 379: 2297–2306.
52. Mack MJ, Lindenfeld J, Abraham WT, et al. 3-year outcomes of transcatheter mitral valve repair in patients with heart failure. J Am Coll Cardiol 2021; 77: 1029–1040.
53. Arnold SV, Stone GW, Jain SS, et al. Prognostic importance of health status versus functional status in heart failure and secondary mitral regurgitation. JACC Heart Fail 2021; 9: 684–692.
54. Ben-Yehuda O, Shahim B, Chen S, Liu M, Redfors B, Hahn RT, et al. Pulmonary hypertension in transcatheter mitral valve repair for secondary mitral regurgitation: the COAPT trial. J Am Coll Cardiol 2020; 76: 2595–2606.
55. Giustino G, Lindenfeld J, Abraham WT, et al. NYHA functional classification and outcomes after transcatheter mitral valve repair in heart failure: the COAPT trial. JACC Cardiovasc Interv 2020; 13: 2317–2328.
56. Hahn RT, Asch F, Weissman NJ, et al. Impact of tricuspid regurgitation on clinical outcomes: the COAPT trial. J Am Coll Cardiol 2020; 76: 1305–1314.
57. Malik UI, Ambrosy AP, Ku IA, et al. Baseline functional capacity and transcatheter mitral valve repair in heart failure with secondary mitral regurgitation. JACC Cardiovasc Interv 2020; 13: 2331–2341.
58. Karam N, Stolz L, Orban M, et al. Impact of right ventricular dysfunction on outcomes after transcatheter edge-to-edge repair for secondary mitral regurgitation. JACC Cardiovasc Imaging 2021; 14: 768–778.
59. Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med 2018; 379: 2307–2318.
60. Lindenfeld J, Abraham WT, Grayburn PA, et al. Association of effective regurgitation orifice area to left ventricular end-diastolic volume ratio with transcatheter mitral valve repair outcomes: a secondary analysis of the COAPT trial. JAMA Cardiol 2021; 6: 427–436.
61. Iung B, Messika-Zeitoun D, Boutitie F, Trochu JN, Armoiry X, Maucort-Boulch D, et al. Characteristics and outcome of COAPT-eligible patients in the MITRA-FR trial. Circulation 2020; 142: 2482–2484.
62. Messika-Zeitoun D, Iung B, Armoiry X, et al. impact of mitral regurgitation severity and left ventricular remodeling on outcome after MitraClip implantation: results from the Mitra-FR trial. JACC Cardiovasc Imaging 2021; 14: 742–752.
63. Kar S, Mack MJ, Lindenfeld J, et al. Relationship between residual mitral regurgitation and clinical and quality-of-life outcomes after transcatheter and medical treatments in heart failure: COAPT trial. Circulation 2021; 144: 426–437.
64. Bedogni F, Popolo Rubbio A, Grasso C, et al. Italian Society of Interventional Cardiology (GIse) registry Of Transcatheter treatment of mitral valve regurgitaTiOn (GIOTTO): impact of valve disease aetiology and residual mitral regurgitation after MitraClip implantation. Eur J Heart Fail 2021; 23: 1364–1376.
65. Reichart D, Kalbacher D, Rubsamen N, et al. The impact of residual mitral regurgitation after MitraClip therapy in functional mitral regurgitation. Eur J Heart Fail 2020; 22: 1840–1848.
66. Higuchi S, Orban M, Stolz L, et al. Impact of residual mitral regurgitation on survival after transcatheter edge-to-edge repair for secondary mitral regurgitation. JACC Cardiovasc Interv 2021; 14: 1243–1253.
67. Chikwe J, O’Gara P, Fremes S, et al. Mitral surgery after transcatheter edge-to-edge repair: society of thoracic surgeons database analysis. J Am Coll Cardiol 2021; 78: 1–9.
68. Simonato M, Whisenant B, Ribeiro HB, et al. Transcatheter mitral valve replacement after surgical repair or replacement: comprehensive midterm evaluation of valve-in-valve and valve-in-ring implantation from the VIVID registry. Circulation 2021; 143: 104–116.
69. Whisenant B, Kapadia SR, Eleid MF, et al. One-year outcomes of mitral valve-in-valve using the SAPIEN 3 transcatheter heart valve. JAMA Cardiol 2020; 5: 1245–1252.
70. Freitas-Ferraz AB, Bernier M, Vaillancourt R, et al. Safety of transesophageal echocardiography to guide structural cardiac interventions. J Am Coll Cardiol 2020; 75: 3164–3173.
71. Zhan Y, Debs D, Khan MA, Nguyen DT, et al. Natural history of functional tricuspid regurgitation quantified by cardiovascular magnetic resonance. J Am Coll Cardiol 2020; 76: 1291–1301.
72. Dreyfus J, Flagiello M, Bazire B, et al. Isolated tricuspid valve surgery: impact of aetiology and clinical presentation on outcomes. Eur Heart J 2020; 41: 4304–4317.
73. Gammie JS, Chu MWA, Falk V, et al. Concomitant tricuspid repair in patients with degenerative mitral regurgitation. N Engl J Med;
https://doi.org/10.1056/NEJMoa2115961. Published online ahead of print 13 November 2021.
74. Montalto C, Sticchi A, Crimi G, et al. Functional and echocardiographic improvement after transcatheter repair for tricuspid regurgitation: a systematic review and pooled analysis. JACC Cardiovasc Interv 2020; 13: 2719–2729.
75. Stocker TJ, Hertell H, Orban M, et al. Cardiopulmonary hemodynamic profile predicts mortality after transcatheter tricuspid valve repair in chronic heart failure. JACC Cardiovasc Interv 2021; 14: 29–38.
76. Duval X, Le Moing V, Tubiana S, et al. Impact of systematic whole-body 18F-fluorodeoxyglucose PET/CT on the management of patients suspected of infective endocarditis: the prospective multicenter TEPvENDO study. Clin Infect Dis 2021; 73: 393–403.
77. Barca L V, Vidal-Bonnet L, Farinas MC, et al. Analysis of sex differences in the clinical presentation, management and prognosis of infective endocarditis in Spain. Heart 2021; 107: 1717–1724.
78. Mentias A, Saad M, Desai MY, et al. Transcatheter versus surgical aortic valve replacement in patients with rheumatic aortic stenosis. J Am Coll Cardiol 2021; 77: 1703–1713.
79. Del Val D, Abdel-Wahab M, Mangner N, et al. Stroke complicating infective endocarditis after transcatheter aortic valve replacement. J Am Coll Cardiol 2021; 77: 2276–2287.
80. McElhinney DB, Zhang Y, Aboulhosn JA, et al. Multicenter study of endocarditis after transcatheter pulmonary valve replacement. J Am Coll Cardiol 2021; 78: 575–589.
81. Alkhouli M, Alqahtani F, Simard T, et al. Predictors of use and outcomes of mechanical valve replacement in the United States (2008– 2017). J Am Heart Assoc 2021; 10: e019929.
82. Jawitz OK, Wang TY, Lopes RD, et al. Rationale and design of PROACT Xa: a randomized, multicenter, open-label, clinical trial to evaluate the efficacy and safety of apixaban versus warfarin in patients with a mechanical On-X Aortic Heart Valve. Am Heart J 2020; 227: 91–99.
83. Zhang B, Salaun E, Côté N, Wu Y, Mahjoub H, Mathieu P, et al. Association of bioprosthetic aortic valve leaflet calcification on hemodynamic and clinical outcomes. J Am Coll Cardiol 2020; 76: 1737–1748.
84. Kwiecinski J, Tzolos E, Cartlidge TRG, et al. Native aortic valve disease progression and bio-prosthetic valve degeneration in patients with transcatheter aortic valve implantation. Circulation 2021; 44: 1396–1408.
85. Christersson C, James SK, Lindhagen L, et al. Comparison of warfarin versus antiplatelet therapy after surgical bio-prosthetic aortic valve replacement. Heart 2020; 106: 838–844.
86. Guimaraes HP, Lopes RD, de Barros ESPGM, et al. Rivaroxaban in patients with atrial fibrillation and a bio-prosthetic mitral valve. N Engl J Med 2020; 383: 2117–2126.